Switzerland (Head Quarters)
IDR Medical Switzerland
Austrasse 95, CH-4051 Basel, Switzerland
T:
+41 (0) 61 535 1109
UK
IDR Medical UK
Unit 104 Eagle Tower, Eagle Tower
Montpellier Drive, Cheltenham, GL50 1TA
T:
+44 (0) 1242 696 790
USA
IDR Medical North America
225 Franklin Street, 26th Floor
Boston, Massachusetts 02110, USA
T:
+1 (0) 617.275.4465

The UK Hospital Landscape
In this blog, our international healthcare consultancy experts explore the UK hospital landscape in detail, and how this should be considered in light of your upcoming market research projects.
Almost all specialist physicians in the UK work in hospitals
Patients typically require a referral from their GP to access this higher level of care, except in urgent or emergency cases. This is also typical for patients who wish to access private healthcare, with insurers and providers often asking for referral from a GP first.
There are 1,229 hospitals in the UK. This number includes the NHS Trust-managed hospitals, and the additional private hospitals that are currently in use.
To fully explore the hospital landscape, it is important to first understand the context in which healthcare is delivered
The UK operates a publicly funded healthcare system, free at the point of care. It is composed of four distinct health systems, with each of the devolved nations responsible for the planning and delivery of their own health services.
While fundamentally similar in many ways, organisational and reimbursement structures differ between them.
These health systems are broken down by the UK’s four nations:
1. England
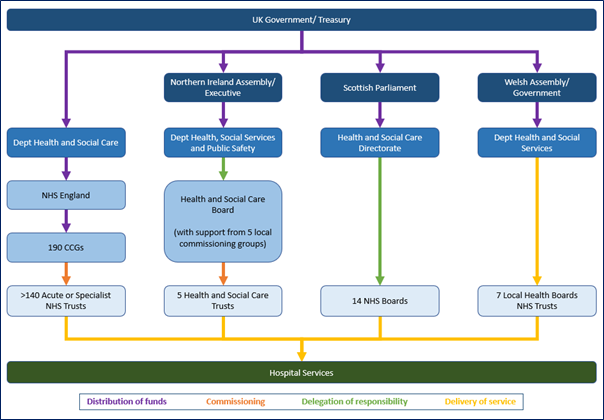
NHS England is the largest health system in the UK, responsible for a population of around 56 million people. The Department of Health and Social Care for the UK is responsible for allocating funds to NHS England.
Healthcare in England operates using internal market principles, whereby different NHS organisations act as either purchasers or providers of health services. It also allows private companies the opportunity to compete to provide services within the NHS.
Under the current system, NHS England distributes funds between 190 Clinical Commissioning Groups (CCGs), as well as directly commissioning some specialist services.
CCGs are local organisations, responsible for planning and commissioning care from service providers, including hospital services from more than 130 Acute or Hospital NHS Trusts.
The NHS in England has undergone numerous reforms over the last two decades, the most recent of which is the introduction of Integrated Care Systems (ICSs). This latest reform is an attempt to better manage coordination of patients across different care areas and reduce the use of hospital services.
ICSs are also likely to take over the role of commissioning from the CCGs, which are expected to be abolished in April 2022.
However, despite interest in care being moved out of hospitals, the UK government has committed to the building and refurbishment of 48 hospitals by 2030 (although this includes some already in the process of being built).
2. Scotland
Each of the administrations in Scotland, Wales, and Northern Ireland receive an annual budget for the provision of devolved public services from the UK Treasury. These administrations have the freedom to decide how they allocate that budget between their departments.
In Scotland, the Health and Social Care Directorate is the parliamentary body overseeing healthcare. They delegate responsibility to NHS Scotland, which is made up of 14 regionally defined NHS Boards, seven Special NHS Boards, and Healthcare Improvement Scotland.
Unlike England, Scotland no longer operates using internal market principles, with the NHS Boards responsible for both the planning and provision of health care.
3. Wales
Wales adopts a similar system to Scotland in that they do not make use of internal market structures. The Department of Health and Social Services develop targets for healthcare in the country, and NHS Wales plans and provides services through seven Local Health Boards (LHBs) and three NHS Trusts.
The LHBs are responsible for hospital care in Wales, although one NHS Trust is responsible for specialist cancer care, and the seven LHBs collaborate to provide other specialist care nationally. LHBs also coordinate with a number of other organisations and public service providers.
4. Northern Ireland
While still considered part of the UK national health service, Health and Social Care (HSC) is the healthcare system in operation in Northern Ireland. Here, the Department for Health, Social Services and Public Safety delegates responsibility for commissioning care to the HSC Board.
Like England, Northern Ireland utilises an internal market structure, however due to a very small population and limited private sector, competition to provide services is low.
Five Local Commissioning Groups (LCGs) make up subcommittees of the HSC Board and are responsible for regional health planning and securing health services that meet local needs.
Five HSC Trusts are then commissioned to provide health and social care in the region. The HSC Trusts have the same geographical boundaries as the LCGs and provide all care, including hospital services.
Reimbursement
In Scotland, Wales, and Northern Ireland, block contracts are the main payment system for health services. The 14 NHS boards (Scotland), seven LHBs (Wales), and five HSC trusts (Northern Ireland) are each allocated fixed budgets based on predicted costs for their region.
They then have the autonomy to manage their budgets, of which hospital services are included.
England on the other hands utilises a national tariff, known as the payment by results system. Hospital services are given a price value and assigned an HRG code. Hospitals submit patient codes upon discharge and commissioners (i.e., the CCGs) will pay the hospitals based on their activity.
Hospital Demographics
There is little data available on the number and type of hospitals in the UK.
However, each country catalogues the hospitals managed under the NHS, which in England, Scotland, and Wales includes NHS run mental health facilities and hospices.
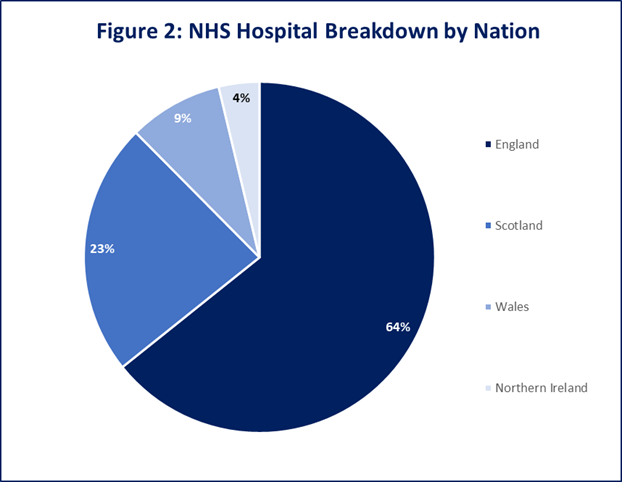
In total, NHS hospitals account for the vast majority of the hospitals in the UK, almost two thirds of which are in England:
Trusts or boards that manage hospitals in all four nations are typically responsible for managing numerous hospitals in a local area.
Teaching is managed this way, too; trusts or boards partner with universities to provide teaching throughout the hospitals they manage. More than 40 trusts or boards have links to medical schools in the UK.
Private Sector
The NHS is responsible for most hospital care in the UK, however it does have a small private sector, with around 11% of the population taking out voluntary private health insurance. Most facilities classified as private hospitals in the UK are independently run mental health services or hospices.
There is also a reasonable level of overlap between private services and those provided by the NHS; most private hospitals do not have the acute capacities of NHS hospitals, and will therefore provide some services through them.
Furthermore, around half of UK physicians offer private healthcare, many alongside their position in the NHS.
Additionally, more so in England than the other nations, the NHS will sometimes contract private hospitals to deliver services to patients, typically where there are long waiting lists; approximately 8% of CCG spending on hospitals is thought to go to private providers.
In conclusion, the nature of the UK hospital landscape is complex
The devolution of health services along with ongoing reforms present a challenge in staying up to date with the latest key stakeholders and opinion leaders.
As an international healthcare consultancy with global reach, we have a lot of experience conducting research in the UK, and can help you access the right stakeholders for your next market research project.
If you would like an initial telephone discussion, or an online meeting to understand how our international healthcare consultancy can help your device take market share, please contact us here.

